Fibromyalgia Testing - CAM 272
Description
Fibromyalgia is a chronic diffuse pain condition and the most common cause of chronic widespread musculoskeletal pain.1 It is also known by “diffuse myofascial pain syndrome,” “fibromyalgia-fibromyositis syndrome,” or “fibromyalgia syndrome.”2 FM has The etiology and pathophysiology of FM is generally unknown, but it can be found with “fatigue, cognitive disturbance psychiatric symptoms, and multiple somatic symptoms;” however, presentation may vary from patient to patient.1,3 Controversy has arisen regarding the disease origin, as it has been considered to be psychogenic or psychosomatic, but recent research indicates it as a disorder of pain regulation, a form of “central sensitization.”1
Terms such as male and female are used when necessary to refer to sex assigned at birth.
Regulatory Status
A search for “Fibromyalgia” on Jan. 7, 2021 yielded 0 lab testing results. A search for any specific tests of the genes likely implicated in FM also did not yield any lab testing results. Additionally, many labs have developed specific tests that they must validate and perform in house. These laboratory-developed tests (LDTs) are regulated by the Centers for Medicare & Medicaid (CMS) as high-complexity tests under the Clinical Laboratory Improvement Amendments of 1988 (CLIA ’88). As an LDT, the U.S. Food and Drug Administration has not approved or cleared this test; however, FDA clearance or approval is not currently required for clinical use (FDA, 2018).
Policy
Application of coverage criteria is dependent upon an individual’s benefit coverage at the time of the request.
The following does not meet coverage criteria due to a lack of available published scientific literature confirming that the test(s) is/are required and beneficial for the diagnosis and treatment of a patient’s illness.
- For the diagnosis of fibromyalgia or chronic pain syndromes, the following tests is considered NOT MEDICALLY NECESSARY:
- Genetic testing (e.g., mutation analysis, copy number variants, epigenetic analysis, mRNA expression, miRNA expression)
- Biomarker panel testing with proprietary algorithms and/or index scores (e.g., FM/a®, NutrEval FMV®).
Table of Terminology
| Term |
Definition |
| 5HT |
Serotonin |
| 5-HT2A |
Serotonin 2A |
| A1AT |
Alpha-1 antitrypsin |
| AAPT |
ACTTION-APS Pain Taxonomy |
| ACE I/D |
Angiotensin-converting enzyme I/D polymorphism |
| ACR |
American College of Rheumatology |
| ACTTION |
Analgesic, Anesthetic, and Addiction Clinical Trial Translations Innovations Opportunities and Networks |
| ADRA1A |
Adrenoreceptor alpha 1A gene |
| ADRB2 |
Adrenoreceptor beta 2 gene |
| ADRB3 |
Adrenoreceptor beta 3 gene |
| AMPA |
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid |
| ANS |
Autonomic nervous system |
| APS |
American Pain Society |
| BDNF |
Brain derived neurotrophic factor gene |
| CB-1 |
Cannabinoid receptor type 1 |
| CLIA ’88 |
Clinical Laboratory Improvement Amendments Of 1988 |
| CMS |
Centers for Medicare & Medicaid Services |
| CNR1 |
Cannabinoid receptor 1 gene |
| CNS |
Central nervous system |
| CNV |
Copy number variant |
| COMT |
Catecholamine o-methyl transferase gene |
| CRA |
Canadian Rheumatology Association |
| CRP |
C-reactive protein |
| CSF |
Cerebrospinal fluid |
| CWP |
Chronic widespread pain |
| DNA |
Deoxyribonucleic acid |
| DRD3 |
Dopamine receptor D3 gene |
| EDN1 |
Endothelin 1 gene |
| ESR |
Erythrocyte sedimentation rate |
| FDA |
Food and Drug Administration |
| FIQ |
Fibromyalgia-Impact Questionnaire |
| FM |
Fibromyalgia |
| GABRB3 |
Gamma-aminobutyric acid receptor subunit beta-3 gene |
| GBP1 |
Guanylate binding protein 1 gene |
| GCH1 |
Guanosine triphosphate (GTP) cyclohydrolase 1 gene |
| GERD |
Gastroesophageal reflux disease |
| GRIA4 |
Glutamate ionotropic receptor AMPA type subunit 4 gene |
| HLA-DRB1 |
Human leukocyte antigen DR beta 1 gene |
| HTR2A |
5-Hydroxytryptamine Receptor 2A gene |
| HTR3A |
5-Hydroxytryptamine Receptor 3A gene |
| HTR3B |
5-Hydroxytryptamine Receptor 3B gene |
| IBS |
Irritable bowel syndrome |
| IFN-γ |
Interferon-γ |
| IGHV1OR21-1 |
Immunoglobulin domain-containing like protein |
| IGLV3-25 |
Immunoglobulin lambda variable 3-25 |
| IL-10 |
Interleukin-10 |
| IL1RAP |
Interleukin-1 receptor accessor protein |
| IL-4 |
Interleukin-4 gene |
| IL-5 |
Interleukin-5 |
| IL-6 |
Interleukin-6 |
| IL-8 |
Interleukin-8 |
| LDTs |
Laboratory-developed tests |
| MAOA |
Monoamine oxidase A gene |
| MAPK |
Mitogen-activated protein kinase |
| MCP-1 |
Monocyte chemoattractant protein-1 |
| MEFV |
Mediterranean fever gene |
| METTL18 |
Methyltransferase-like 18 |
| MIP-1β |
Macrophage inflammatory protein-1β |
| MSP |
Multisite pain |
| MTHFR |
Methylenetetrahydrofolate reductase gene |
| MYT1L |
Myelin transcription factor 1 like gene |
| NA |
Noradrenaline |
| NRXN3 |
Neurexin 3 gene |
| OPRM1 |
Opioid receptor mu 1 gene |
| PBMC |
Plasma and peripheral blood mononuclear cells |
| PHA |
Phytohemagglutinin |
| PMA |
Phorbol-12-myristate-13-acetate |
| RA |
Rheumatoid arthritis |
| RGS4 |
Regulator of G protein signaling 4 gene |
| SCL-90 |
Symptom Checklist-90 for Psychopathological Disorders |
| SCN9A |
Sodium voltage-gated channel alpha subunit 9 gene |
| SLC64A4 |
Solute carrier family 64 member 4 gene |
| SERPINA1 |
Serpin family A member 1 gene |
| SLE |
Systemic lupus erythematosus |
| SNPs |
Single nucleotide polymorphisms |
| SS |
Sjögren syndrome |
| TAAR1 |
Trace amine-associated receptor 1 gene |
| TACR1 |
Tachykinin receptor 1 gene |
| TMD |
Temporomandibular joint disorder |
| TPC |
Tender point count |
| TPQ |
Tridimensional Personality Questionnaire |
| TRPV2 |
Transient receptor potential vanilloid channel 2 gene |
| TRPV3 |
Transient receptor potential vanilloid channel 3 gene |
| TSH |
Thyroid stimulating hormone |
| TSPO |
Translocator protein gene |
| WPI |
Widespread pain index |
Rationale
Fibromyalgia (FM) is a condition characterized by chronic and diffuse non-inflammatory musculoskeletal pain. FM is often accompanied by fatigue, cognitive disturbances (“fibro fog”), psychiatric symptoms, and multiple other nonspecific somatic symptoms.1,4 Aside from the secondary symptoms, patients may at times experience abdominal and chest wall pain, irritable bowel syndrome (IBS), gastroesophageal reflux disease (GERD), and symptoms of autonomic nervous system (ANS) dysfunction. Despite this, FM is generally of unknown etiology and pathophysiology. However, FM should be considered as a diagnosis in patients experiencing idiopathic chronic pain for at least three months and is solely confirmed by a clinical, symptom-based assessment.5
What adds to the controversial and mysterious nature of the condition is that it depends on subjective symptoms. On a normal physical examination, patients often appear well and do not show abnormalities other than “widespread soft tissue tenderness” with normal laboratory and radiologic studies, making it a common but elusive diagnosis. However, a history of other medical conditions that cause musculoskeletal pain can coexist with or mimic FM like rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and thyroid disease. Medical history can support a FM diagnosis.1 FM is more commonly diagnosed in women than men. The prevalence of FM in the United States and other countries is about two to three percent and incidence tends to increase with age.6 FM can also be diagnosed in adolescents in the form of juvenile primary fibromyalgia, and it is confirmed mostly symptomatically but based on slightly different diagnostic criteria for research and epidemiological purposes.3
Fibromyalgia is categorized as a “disorder of pain regulation,” under “central sensitization.”7 This finding is supported by biochemical abnormalities that are oftentimes present in FM patients: low concentrations of metabolites of serotonin (5HT) and noradrenaline (NA), and high concentrations of substance P and nerve growth factors.8 Patients are more sensitive to central nervous system inputs of pain, and those with FM at times can experience symptoms like those suffering from other central pain disorders, like migraines, IBS, and temporomandibular joint disorder (TMD).7 Reduced 5HT and NA may actually account for the widespread pain symptoms by contributing to the dysfunction of endogenous systems that inhibit pain sensation.8
Contrary to the established findings published about FM, recent research has demonstrated that there is a possible genetic basis to the disease progression; up to 50% of disease risk can be attributed to candidate genes.5 There also appears to be a strong familial predisposition to FM, although it is suspected to have a more polygenic mode of inheritance.9,10 However, there is no singular definitive gene that directly causes FM; several genes under consideration include SLC64A4, TRPV2, MYT1L, and NRXN3.5 Single nucleotide polymorphisms (SNPs) in the SLC64A4 gene, which encodes a sodium-dependent serotonin transporter, has been associated with both FM and TMD. SLC64A4 mutations that cause increased serotonin reuptake have been associated with high levels of depression and psychological disorders, as well as “SCL-90 [Symptom Checklist-90 for psychopathological disorders] scores for somatic awareness and anger, TPQ [tridimensional personality questionnaire] harm avoidance trait, increased salivary cortisol level, [and] increased leukocyte count.”5,11 TRPV2 (transient receptor potential vanilloid channel 2) gene is needed for not only cell cycle progression, growth, and differentiation of hematopoietic stem cells and innate immunity, but also the pain threshold due to its presence in the mechanoresponsive and thermo-responsive neurons in the dorsal root and trigeminal ganglia.5,12,13 Genetic correlations in FM between mutations in SLC6A4 and TRPV2, which encodes a calcium-permeable channel that is heat-activated and modulates many cellular functions, are further supported by linkage analysis done with FM to the chromosome 17p11.2-q11.2 region, which happens to house the two genes.14,15
Docampo, et al. (2014) discovered that the rs11127292 polymorphism in the MYT1L (myelin transcription factor 1 like) gene, which is critical in the process of neuronal differentiation and has historically been associated with neuropsychiatric disorders, and an intronic CNV (copy number variant) in the NRXN3 (neurexin 3) gene, which is involved in signal transmission by promoting synapse stability and function, affect the central nervous system (CNS) aspect of FM as well.16
Studies have also examined the differences in other allelic frequencies and influence of genetics on the sequelae of FM progression. Smith, et al. (2012) identified significant variations in allelic frequency of GABRB3 (rs4906902), TAAR1 (rs8192619), and GBP1 (rs7911) between FM patients and controls. TAAR1 was demonstrated to alter dopamine bioavailability and function, which may cause the increased pain sensitivity seen in FM. RGS4, CNR1, and GRIA4 were implicated in other cohorts from the study by Smith, et al. (2012) and are genes primarily involved in mechanisms of analgesia and central sensitivity as well. RGS4, which is expressed in the CNS regions like the dorsal horn of the spinal cord and the locus coeruleus, influences opioid receptor function when overexpressed. CNR1, which encodes the CB-1 cannabinoid receptor, has been indirectly utilized in FM treatment by the cannabinoid receptor agonist nabilone. Low CNR1 expression and thus low CB-1 receptor activity may pose as a strong candidate for future testing, as several FM patients have increased circulating anandamide, an endocannabinoid, which has been hypothesized to underlie the pain in conditions like FM. Alterations to the GRIA4 gene affect AMPA (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid) receptors, which play roles in the pain and comorbidities associated with FM.17
Another gene commonly associated with FM is the COMT (catecholamine o-methyl transferase) gene. Though not directly affecting disease presentation, the V158M variant may contribute to subsequent depression, anxiety, and disability in many FM females.5 Mutations in the COMT gene are more closely linked to “pain catastrophizing, increased pain level during elevated pain attention, thermal and pressure sensitivity, psychological distress, increase number of tender points in TPC [tender point count], pain and positive affect interaction, and FIQ [fibromyalgia-impact questionnaire]-defined pain, fatigue, sleep, disturbance, morning stiffness, and disability.”11 Similarly, mutations in the HTR2A (5-hydroxytryptamine receptor 2A) gene, which encodes for its receptor, 5-HT2A, contributed to lower levels of total 5-HT in serum and CSF of FM patients.18 The phenotype in FM more closely relates to psychological facets of FM – including reduced perception of environmental quality, “increased SCL-90-R total score and subscales scores for somatic awareness, anxiety, psychosis, obsessive-compulsive behavior, hostility, global severity index, interpersonal sensitivity, phobic anxiety, [and] depression.”11
Research has also demonstrated the role of epigenetics in FM phenotype and progression. Ciampi de Andrade, et al. (2017) investigated DNA methylation states in samples obtained from FM cases and healthy controls, and found that the majority (1042 genes, 65%) of the differently methylated genes between the two were mostly hypomethylated. These genes were involved in “transduction and calcium signaling, MAPK signaling pathway, regulation of actin cytoskeleton endocytosis, and neuroactive ligand-receptor interaction pathways,” and the sites that were identified were involved in DNA repair, immune system response and regulation, and membrane transport.5 Additionally, circulating miRNAs obtained from cerebrospinal fluid (CSF) and serum samples were found to be associated with many of the clinical symptoms of FM, including pain and fatigue, alterations in energy metabolism and growth, alterations in pain threshold, and sleep disturbance.20,21
Proprietary Testing
Some researchers have opted for a proteomics approach to identify individuals with FM. Among females with FMS, Han, et al. (2020) discovered dysregulated proteins and mechanisms associated with an FM diagnosis. They propose a panel of methyltransferase-like 18 (METTL18), immunoglobulin lambda variable 3-25 (IGLV3-25), interleukin-1 receptor accessor protein (IL1RAP), and putative V-set and immunoglobulin domain-containing like protein (IGHV1OR21-1) to differentiate FM from healthy controls. This conclusion was drawn from using a decision tree model that yielded an accuracy of 0.97. Collectively, they offered 100% detection sensitivity in their training cohort, and a specificity of 88%.22
Genova Diagnostics has also released the NutrEval FMV® Profile, which is a “blood and urine profile that evaluates over 125 biomarkers and assesses the body's functional need for 40 antioxidants, vitamins, minerals, essential fatty acids, amino acids, digestive support, and other select nutrients.” NutrEval® aims to provide insight into conditions such as depression, anxiety, certain inflammatory conditions, and chronic pain syndromes.23 While there are no peer-reviewed studies published to confirm either the analytical or clinical utility of this particular proprietary test, researchers have delved into the biomarkers that comprise this assay. The aforementioned research on COMT proves relevant in the genomics component of this test. The clinical utility for the NutrEval® Profile is particularly pertinent to the chronic pain aspect. In patients with chronic pain, it was found that quinolinic acid, pyroglutamic acid (indicator of glutathione depletion), xanthurenic acid (indicator of vitamin B6 insufficiency), 3-hydroxyropyl mercapturic acid (acrolein metabolite), and methylmalonic acid (indicator of vitamin B12 deficiency) were all elevated to a certain degree among patients experiencing chronic pain. Seventy-seven percent of patients with chronic pain all had at least one abnormal biomarker.24 This demonstrates that understanding the role of nutrition metabolism is necessary for delineating the underlying processes of FM, a chronic pain condition, but additional research is needed.
Clinical Utility and Validity
Currently, most, if not all, of the FM diagnoses are solely clinical. Judgment is made subjectively and dependent on guidelines to conclude if subjective symptoms translate to FM. The sensitivity and specificity of utilizing the 2016 ACR guidelines, when compared to the 1990 criteria in a referral care setting, are 71% and 60%, respectively, with a positive predictive value of 85% and a negative predictive value of 39%.25 These statistical measures evidently prove that there need be more sensitive and specific measures beyond clinical symptoms for diagnosis of FM.
The clinical utility of an FM diagnosis extends beyond genetic testing and biomarkers; FM is also found concurrently among those with primary immunodeficiency and autoimmune diseases, such as RA, SLE, and Sjögren Syndrome (SS).22,26 Confirming an FM diagnosis could aid in explicating the additional complications found in RA and SLE, such as “alternating constipation and diarrhea, urinary frequency, diffuse paresthesias, and cognitive difficulties.” The converse also holds true – diagnoses of SS could prompt possible FM diagnoses as well, as seen in the cases of seeing sicca symptoms and TPC of six (though not necessary with 2016 ACR guidelines).26
Janssen, et al. (2021) conducted a review that identified the polymorphisms related to FM and the respective clinical characteristics. From 27 articles, they found the relevant genes to be MTHFR, RGS4, MYT1L, TACR1, SCN9A, DRD3, ADRB2, IL-4, HLA-DRB1, EDN1, CNR1, TAAR1, OPRM1, ADRA1A, ADRB3, BDNF, GRIA4, HTR3A, HTR3B, HTR2A, SERPINA 1 or A1AT, NRXN3, GCH1, MEFV, TRPV3, SLC6A4, ACE I/D, TSPO, COMT, and MAOA. Additionally, “73.33% of the genes related to FM were also associated with some psychological disorders, such as anxiety, depression, schizophrenia, and obsessive and compulsive disorder, and 40.00% with pain sensitivity and/or migraine, besides other disorders associated (drug addiction, autoimmune disorders, circulatory problems, and metabolic alterations).” Of note, SLC6A4, HTR3A, HTR3B, and HTRA genes were associated with serotonergic regulation, chronic pain conditions, and anxiogenic situations; COMT was related to FM risk and increase in pain severity, increased likelihood of psychological disorders like depression, anxiety and schizophrenia, alcoholism, opioid addiction, and eating disorders; BDNF was associated with hyperalgesia in FM; and TACR1 was related to dementia and fatigue. As for treating FM, Janssen, et al. (2021) also found that TAAR1, RGS4, CNR1, GRIA4 may be considered as targets. These collective findings continue to demonstrate the comorbidities associated with FM, and how understanding the genetic bases may aid in preventing and treating additional sequelae.27
Kendler, et al. (2022) studied the familial genetic risk for functional somatic disorders including internalizing disorders, chronic fatigue syndrome, IBS, and FM. The study included 5,829,186 individuals in Sweden. The authors used a novel method that assessed aggregated risk in first to fifth degree relatives and adjusted for cohabitation. “Patients with FM carry substantial genetic risks not only for FM, but also for pain syndromes and internalizing, autoimmune and sleep disorders.” Overall, patients with FM had a unique family risk genetic score with elevated genetic risk across other disorders; the was a similar but less marked pattern of genetic risks in patients of other functional somatic disorders. The authors suggest that the genetic risk score for FM differentiated it from classic autoimmune disorder and internalizing disorder.28
American Pain Society
The Analgesic, Anesthetic, and Addiction Clinical Trial Translations Innovations Opportunities and Networks (ACTTION) partnership with the Food and Drug Administration (FDA) and APS created the ACTTION-APS Pain Taxonomy (AAPT) to help standardize clinically useful and consistent diagnoses of chronic pain disorders. First and foremost, all patients must have chronic pain to be diagnosed with FM. The working group members raised a concern of defining FM-pain as by the 1990 ACR criteria (CWP – chronic widespread pain) or the ACR 2010/2016 criteria of multisite pain (MSP), which were distinguished in count (MSP) versus anatomical distribution (CWP) of pain.
To facilitate identifying FM in clinical practice and in research, the AAPT core diagnostic criteria for FM are as follows:
- “MSP defined as 6 or more pain sites from a total of 9 possible sites [head; left arm; right arm; chest; abdomen; upper back and spine; lower back and spine, including buttocks; left leg; and right leg]
- Moderate to severe sleep problems OR fatigue
- MSP plus fatigue or sleep problems must have been present for at least 3 months.”9
This guideline did not mention genetic testing for FM.9
American College of Rheumatology (ACR)
In 2016, the ACR published revisions to their 2010/2011 guidelines on preliminary diagnostic criteria for fibromyalgia and measurements of symptom severity. To satisfy a diagnosis of fibromyalgia, a patient must have:
- “Widespread pain index (WPI) ≥ 7 and symptom severity (SS) scale score ≥ 5 or WPI 4-6 and SS scale score ≥ 9.
- Generalized pain, defined as pain in at least 4 or 5 regions, must be present. Jaw, chest, and abdominal pain are not included in generalized pain definition.
- Symptoms have been present at a similar level for at least 3 months.
- A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses.”
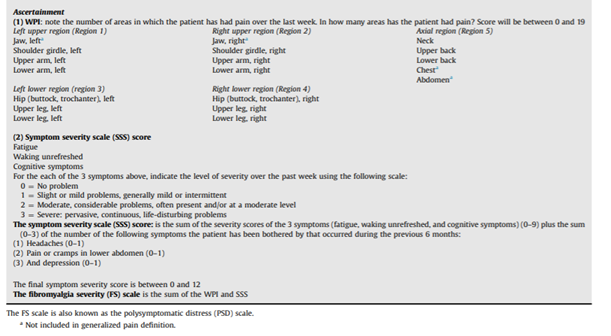
The table below obtained from the ACR’s publication regarding ascertainment of WPI and SS is shown.
Several cases previously deemed positive by the 2010/2011 criteria would be considered negative by the 2016 modified criteria, indicating a lower specificity. The current criteria also state patients can experience pain in 4-5 regions (four quadrants and axial), termed “generalized pain,” to distinguish from the 1990 guideline’s “widespread pain” definition. The 2016 ACR guidelines also now recognize spatial distribution of painful sites.9 It lastly modifies the language from the 2010 guidelines that discuss other disorders serving as the etiology of experienced pain, and assumes the 1990 ACR guideline criterion of possible comorbidities with fibromyalgia (#4).29
After conducting an in-depth review of existing guidelines and literature, Heymann, et al. (2017) published recommendations based on the 2010 ACR guidelines, and endorse using the 2010 ACR criteria for diagnosis of FM. They stated:
- “The presence of widespread pain is essential for the diagnosis of patients with suspected FM.
- Tender points may be useful in the diagnosis of fibromyalgia when evaluated in combination with other functional disorders covered in the 2010 [ACR] criteria. The tender point count may be correlated with the intensity of some symptoms, particularly emotional stress.
- Sleep disorders and changes in cognition and fatigue should be considered in the diagnosis of FM. They should also be considered in the assessment of severity of patients with FM.
We suggest the systematic measurement of mood disorders using validated instruments suitable to the healthcare level in which they are administered because they are highly important when assessing the severity of patients with FM.”30
These guidelines did not mention genetic testing for FM.
Canadian Rheumatology Association (CRA)
The CRA released recommendations to the “identification, evaluation, and management” of those with FM after conducting a needs assessment. In relation to diagnosis of FM, the CRA recommends:
- “Fibromyalgia, a condition that can wax and wane over time, should be diagnosed in an individual with diffuse body pain that has been present for at least 3 months, and who may also have symptoms of fatigue, sleep disturbance, cognitive changes, mood disorder, and other somatic symptoms to variable degree, and when symptoms cannot be explained by some other illness [Level 5, Grade D].
- All patients with a symptom complaint suggesting a diagnosis of fibromyalgia should undergo a physical examination which should be within normal limits except for tenderness on pressure of soft tissues (i.e., hyperalgesia which is increased pain following a painful stimulus) [Level 4, Grade D].
- Fibromyalgia should be diagnosed as a clinical construct, without any confirmatory laboratory test, and with testing limited to simple blood testing including a full blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), creatine kinase, and thyroid stimulating hormone (TSH). Any additional laboratory or radiographic testing should depend on the clinical evaluation in an individual patient that may suggest some other medical condition [Level 5, Grade D].”31
This guideline did not mention genetic testing for FM.31
American Family Physician (AFP)
The AFP published a guideline in 2023 that outlines recommendations for Diagnosis and Management of Fibromyalgia. Recommendations related to diagnosis include:
- Fibromyalgia should be considered in patients that have chronic pain and a history of tissue injury or inflammation that has been present for more than three months; patients must also present with fatigue, mood issues, and sleep disturbances for more than three months.
- The following criteria are all acceptable methods of diagnosis: The 2011 ACR criteria, the 2016 ACR criteria, and the 2019 AAPT criteria.
- Fibromyalgia is a clinical diagnosis and laboratory testing is not needed as a routine measure. However, fatigue can arise from many origins, and providers may consider the following to eliminate other causes: a complete blood count to exclude anemia, a comprehensive metabolic panel and a TSH test. Other tests, such as those for rheumatoid factor or antinuclear antibody levels are “not recommended” in individuals without suspected rheumatologic conditions because these tests can have high false-positive rates.32
References
1. Goldenberg DL. Clinical manifestations and diagnosis of fibromyalgia in adults. UpToDate. Updated Sep 3. Accessed January 3, 2025. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-fibromyalgia-in-adults
2. Ada. Fibromyalgia. Ada Health GmbH. Updated March 15. https://ada.com/conditions/fibromyalgia/
3. Kimura Y, Walco GA. Fibromyalgia in children and adolescents: clinical manifestations and diagnosis. UpToDate. Updated December 20. https://www.uptodate.com/contents/fibromyalgia-in-children-and-adolescents-clinical-manifestations-and-diagnosis
4. Galvez-Sánchez CM, Reyes Del Paso GA. Diagnostic Criteria for Fibromyalgia: Critical Review and Future Perspectives. J Clin Med. 2020;9(4):1219. doi:10.3390/jcm9041219
5. D'Agnelli S, Arendt-Nielsen L, Gerra MC, et al. Fibromyalgia: Genetics and epigenetics insights may provide the basis for the development of diagnostic biomarkers. Mol Pain. Jan-Dec 2019;15:1744806918819944-1744806918819944. doi:10.1177/1744806918819944
6. Bhargava J, Hurley JA. Fibromyalgia. StatPearls. StatPearls Publishing LLC; 2023. https://www.ncbi.nlm.nih.gov/books/NBK540974/
7. Goldenberg DL. Pathogenesis of fibromyalgia. UpToDate. Updated June 12. Accessed June 23, 2025. https://www.uptodate.com/contents/pathogenesis-of-fibromyalgia
8. Julien N, Goffaux P, Arsenault P, Marchand S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain. 2005/03/01/ 2005;114(1):295-302. doi:10.1016/j.pain.2004.12.032
9. Arnold LM, Bennett RM, Crofford LJ, et al. AAPT Diagnostic Criteria for Fibromyalgia. The Journal of Pain. 2019/06/01/ 2019;20(6):611-628. doi:10.1016/j.jpain.2018.10.008
10. Buskila D, Sarzi-Puttini P, Ablin JN. The genetics of fibromyalgia syndrome. Pharmacogenomics. Jan 2007;8(1):67-74. doi:10.2217/14622416.8.1.67
11. Diatchenko L, Fillingim RB, Smith SB, Maixner W. The phenotypic and genetic signatures of common musculoskeletal pain conditions. Nature Reviews Rheumatology. 2013/06/01 2013;9(6):340-350. doi:10.1038/nrrheum.2013.43
12. Santoni G, Farfariello V, Liberati S, et al. The role of transient receptor potential vanilloid type-2 ion channels in innate and adaptive immune responses. Mini Review. Frontiers in Immunology. 2013-February-14 2013;4(34)doi:10.3389/fimmu.2013.00034
13. Mickle AD, Shepherd AJ, Mohapatra DP. Sensory TRP channels: the key transducers of nociception and pain. Prog Mol Biol Transl Sci. 2015;131:73-118. doi:10.1016/bs.pmbts.2015.01.002
14. Arnold LM, Fan J, Russell IJ, et al. The fibromyalgia family study: a genome-wide linkage scan study. Arthritis Rheum. 2013;65(4):1122-1128. doi:10.1002/art.37842
15. Kojima I, Nagasawa M. TRPV2. Handb Exp Pharmacol. 2014;222:247-72. doi:10.1007/978-3-642-54215-2_10
16. Docampo E, Escaramís G, Gratacòs M, et al. Genome-wide analysis of single nucleotide polymorphisms and copy number variants in fibromyalgia suggest a role for the central nervous system. Pain. 2014/06// 2014;155(6):1102-1109. doi:10.1016/j.pain.2014.02.016
17. Smith SB, Maixner DW, Fillingim RB, et al. Large candidate gene association study reveals genetic risk factors and therapeutic targets for fibromyalgia. Arthritis Rheum. Feb 2012;64(2):584-93. doi:10.1002/art.33338
18. Park D-J, Lee S-S. New insights into the genetics of fibromyalgia. Korean J Intern Med. 2017;32(6):984-995. doi:10.3904/kjim.2016.207
19. Ciampi de Andrade D, Maschietto M, Galhardoni R, et al. Epigenetics insights into chronic pain: DNA hypomethylation in fibromyalgia-a controlled pilot-study. Pain. Aug 2017;158(8):1473-1480. doi:10.1097/j.pain.0000000000000932
20. Bjersing JL, Lundborg C, Bokarewa MI, Mannerkorpi K. Profile of cerebrospinal microRNAs in fibromyalgia. PLoS One. 2013;8(10):e78762-e78762. doi:10.1371/journal.pone.0078762
21. Bjersing JL, Bokarewa MI, Mannerkorpi K. Profile of circulating microRNAs in fibromyalgia and their relation to symptom severity: an exploratory study. Rheumatol Int. Apr 2015;35(4):635-42. doi:10.1007/s00296-014-3139-3
22. Han C-L, Sheng Y-C, Wang S-Y, Chen Y-H, Kang J-H. Serum proteome profiles revealed dysregulated proteins and mechanisms associated with fibromyalgia syndrome in women. Sci Rep. 2020;10(1):12347-12347. doi:10.1038/s41598-020-69271-w
23. Genova. NutrEval® FMV. Genova Diagnostics. Accessed January 10, 2021. https://www.gdx.net/product/nutreval-fmv-nutritional-test-blood-urine
24. Gunn J, Hill MM, Cotten BM, Deer TR. An Analysis of Biomarkers in Patients with Chronic Pain. Pain Physician. Jan 2020;23(1):E41-e49. doi:10.36076/ppj.2020/23/E41
25. Ahmed S, Aggarwal A, Lawrence A. Performance of the American College of Rheumatology 2016 criteria for fibromyalgia in a referral care setting. Rheumatology International. 2019/08/01 2019;39(8):1397-1403. doi:10.1007/s00296-019-04323-7
26. Wilke WS. The Clinical Utility of Fibromyalgia. JCR: Journal of Clinical Rheumatology. 1999;5(2)
27. Janssen LP, Medeiros LF, Souza A, Silva JD. Fibromyalgia: A Review of Related Polymorphisms and Clinical Relevance. An Acad Bras Cienc. 2021;93(suppl 4):e20210618. doi:10.1590/0001-3765202120210618
28. Kendler KS, Rosmalen JG, Ohlsson H, Sundquist J, Sundquist K. A distinctive profile of family genetic risk scores in a Swedish national sample of cases of fibromyalgia, irritable bowel syndrome, and chronic fatigue syndrome compared to rheumatoid arthritis and major depression. Psychological Medicine. 2022:1-8. doi:10.1017/S0033291722000526
29. Wolfe F, Clauw DJ, Fitzcharles M-A, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Seminars in Arthritis and Rheumatism. 2016/12/01/ 2016;46(3):319-329. doi:10.1016/j.semarthrit.2016.08.012
30. Heymann RE, Paiva ES, Martinez JE, et al. New guidelines for the diagnosis of fibromyalgia. Revista Brasileira de Reumatologia (English Edition). 2017/01/01/ 2017;57:467-476. doi:10.1016/j.rbre.2017.07.002
31. Fitzcharles MA, Ste-Marie PA, Goldenberg DL, et al. Canadian Guidelines for the diagnosis and management of fibromyalgia syndrome. Canadian Rheumatology Association. Updated August 17. Accessed January 3, 2021. https://rheum.ca/wp-content/uploads/2017/11/2012CanadianFMGuidelines_17August2012.pdf
32. Winslow BT, Vandal C, Dang L. Fibromyalgia: Diagnosis and Management. Am Fam Physician. Feb 2023;107(2):137-144.
Coding Section
| Code | Number | Description |
| CPT | 81479 | Unlisted molecular pathology procedure |
| 81599 | Unlisted multianalyte assay with algorithmic analysis | |
| 84999 | Unlisted chemistry procedure |
Procedure and diagnosis codes on Medical Policy documents are included only as a general reference tool for each policy. They may not be all-inclusive.
This medical policy was developed through consideration of peer-reviewed medical literature generally recognized by the relevant medical community, U.S. FDA approval status, nationally accepted standards of medical practice and accepted standards of medical practice in this community, and other nonaffiliated technology evaluation centers, reference to federal regulations, other plan medical policies, and accredited national guidelines.
"Current Procedural Terminology © American Medical Association. All Rights Reserved"
History From 2020 Forward
| 04/10/2025 | Annual review, no change to policy intent. Updating description, rationale, guidelines/recommendations, and references. |
| 04/18/2024 | Annual review, no change to policy intent. Updating description, table of terminology, rationale and references. |
| 04/07/2023 | Annual review, no change to policy intent, but, policy being rewritten for clarity and consistency. Also updating description, rationale and reference. |
| 04/22/2022 |
Annual review, no change to policy intent. Updating rationale and references. Adding table of terminology. |
| 04/07/2021 |
New Policy |