Increasing Access to Behavioral Health Care in the Face of COVID-19
Aug. 6, 2020
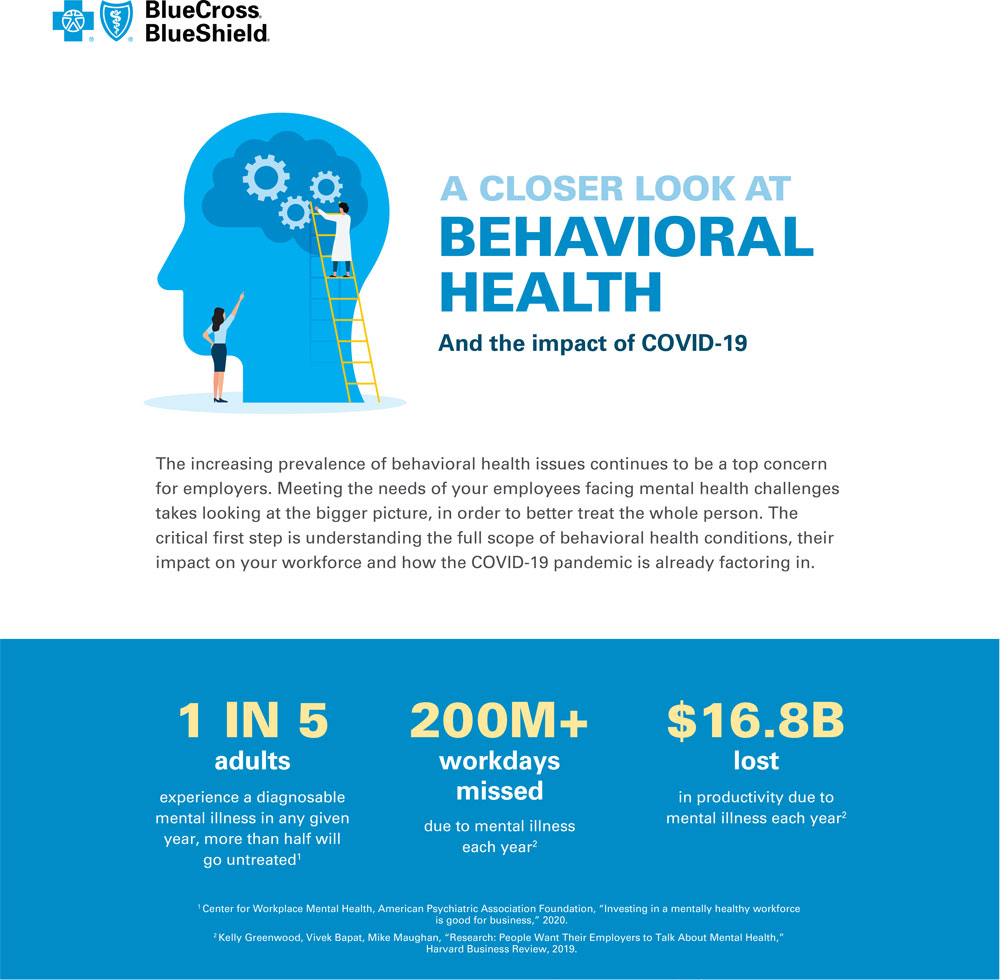
America was in the midst of a behavioral health crisis even before the world had ever heard of COVID-19. Six of the top 10 health conditions affecting millennials — soon to be the majority of the U.S. workforce — are behavioral health conditions. Access to behavioral health care was also in crisis before the pandemic. The leading barriers to care are cost and availability. Not knowing where to find proper care, and not being able to afford it when they do, leads employees who need help to go untreated. In fact, 47 percent of millennials have delayed or avoided medical treatment because of health care costs, according to the Blue Cross Blue Shield Health of America National Generation Survey. And as millennials get older, the cost of treatment — for employers and employees — will only increase.
The pandemic has significantly affected our nation’s mental health. It has created new obstacles for people already struggling with a behavioral health conditions. As the pandemic continues, Americans are reporting increased levels of anxiety and stress. This creates new urgency around providing your employees behavioral health care that’s easier to access and more affordable.
Solving for Siloed Care That Complicates Treatment and Increases Costs
Increase access to integrated care.
Historically, the No. 1 barrier between employees and behavioral health care has been cost, much of which is driven by the siloed nature of our health care system. Increasing access to integrated care is critical, since 68 percent of people with a behavioral health condition also have a secondary underlying health condition, such as heart disease or diabetes. And health care costs for treating employees with behavioral and chronic medical conditions are two to three times higher than for those without behavioral health conditions.
Reevaluate the cost-care relationship.
While it’s true behavioral and physical health are linked and equally important to overall health, behavioral health conditions require more frequent management and check-ins. This means using the same payment structure as we do for physical health can cause costs to stack up quickly. But changing that structure even slightly can have a big impact. A recent study by leading virtual behavioral health care provider AbleTo revealed that just eliminating a $10 copay doubled employee engagement.
Bring more behavioral health in network.
Networks need to provide better access to more behavioral health support. Employers can play a major role in driving this change by asking their health care partner to include in-network providers that offer more integrated, multidimensional care models. They can also work with their health care partners to explore new ways to approach copays and premiums.
Practicing Specialists Are Increasingly Hard to Find
After cost, availability creates another critical barrier to care in terms of provider shortages and challenges related to scheduling and visits. Two out of five Americans live in areas designated by the federal government as having a shortage of behavioral health care providers.
Therapy and substance use disorder treatment are areas of top concern.
More than 60 percent of practicing psychiatrists are over the age of 55 according to data from the Association of American Medical Colleges (AAMC). Meanwhile, the need for treatment is expected to rise. A recent study published in Psychiatric Services revealed that six out of 10 initial phone calls made to outpatient psychiatrists went unanswered. Yet even after two calls, appointments were secured with only about one-quarter of the doctors. The average waiting time for a first visit was 25 days.
When it comes to tackling substance use disorder, drug overdoses are now the leading cause of accidental death in the U.S. And the rising costs of addiction related to crime, lost work productivity and health care exceed $700 billion annually. Substance use disorder is also in the top five behavioral health conditions, yet many treatment centers are out-of-network. This makes them harder to access, afford and know how to evaluate.
COVID-19 Intensifies the Need for Behavioral Health Care
Since the COVID-19 pandemic began, Americans are reporting significant and sustained increases in symptoms of depression and anxiety. Daily routines, both personal and professional, have been upended, increasing physical, mental and financial strain.
These combined stressors create a kind of perfect storm for an increase in the development of mental health conditions. And data in our most recent infographic suggests that negative behavior among millennials has also been rising since the pandemic began.
Download complete infographic here.
Virtual claims for behavioral health services for BlueCross BlueShield of South Carolina have increased more than 3,800 percent. Behavioral health providers who have been approved to be in the BlueCross telehealth network increased from 26 providers in 2019 to 1,371 in 2020, a more than 5,100-percent increase in providers who can continue to provide virtual visits for behavioral health needs.
“We anticipate that many providers will continue to leverage virtual visits after the pandemic has receded and some are moving towards providing primarily virtual visits for the foreseeable future,” says Dr. April Richardson, a medical director with BlueCross.
One thing employers should be exploring with their health care partner is making no-cost screenings standard practice.
Employers Are Bringing Behavioral Health Care Within Reach
Prior to COVID-19, employers, too, were already increasing efforts to make behavioral health care accessible for their employees. Now, they’re ramping up even more. This includes changes in employee assistance programs (EAPs), from discounts on digital care apps to more virtual well-being service options like remote yoga classes.
“More than half of large employers are planning to expand the range of telehealth benefits offered in 2020 to include services such as virtual mental health counseling,” says Ellen Kelsay, president and CEO of the Business Group on Health. As we transition back to the workplace, more large employers may also look to bring clinicians and counselors on-site, she says.
In fact, BlueCross has been doing that. Several employer groups have asked for training or information to share with employees or HR departments on behavioral health issues arising from the COVID-19 pandemic.
Tele-behavioral health and virtual care apps are also a natural fit. These solutions provide convenience for employees through fluid scheduling, easier connections to care professionals and improved access without the stigma of seeking help. From evidence-based cognitive behavioral therapy to resiliency digital tools, these platforms offer multiple ways for employees to connect with practitioners, from live audio and video chat to instant messaging.
BlueCross’ groups have expanded use of these kinds of digital tools to increase access to care for members. By using the apps, the care managers can interact more frequently with the member through their phone in order to better support the member.
“In our behavioral health care management programs, we have seen an increase in the severity of depression symptoms for a significant proportion of our members since the pandemic began. We are working with our members to increase the frequency of contacts and leveraging their benefit options, like access to behavioral health telehealth visits, to help them get the support they need,” Richardson says.
Improving Access: This Is How
Here’s what employers can do to help make powerful change happen and improve their employees’ access to better health care.
Expand resources.
Help employees connect with the care they need by expanding your behavioral health resources and improving access points — from virtual care to on-demand or on-site clinicians and counseling. Ask your health care partner to include and expand in-network providers that offer a multidimensional care model and for resources that help your employees find them.
Make virtual care a priority.
Examine your employees’ virtual care usage since March and consider making changes brought on by the COVID-19 pandemic permanent. Ask your health care partner about resources that can help employees know which ones are right for them.
Get smart about affordability and screenings.
Explore ways with your health care partner to lower or remove copays when it comes to behavioral health, where check-ins are needed more often. Also, make no-cost screenings standard, similar to preventive care — to create stigma-free dialogue with a professional who can explain results and help employees find the right assistance.
Drive awareness.
Foster a deeper understanding of the connection between behavioral health care and physical health care and use internal communications to promote the quality, affordability and effectiveness of available resources.
The Center for Workplace Mental Health, American Psychiatric Association, and the Harvard Business Review are independent organizations that offer health information you may find helpful.
 The Importance of Building a Network During a Pandemic
The Importance of Building a Network During a Pandemic
Because of the pandemic, many South Carolinians have found there has been a shift in employment, opportunities and career growth. Business networking remains an important tool for working professionals, whether looking for a new job after losing one, staying updated with business trends or connecting for career advancement. Experts from the Charleston Metro Chamber of Commerce offer insight into building a professional network today.
Read MoreRelated Reading:




















