Dental Frequently Asked Questions
Is there a designated Provider Advocate for dental services?
No, there is not a specific Provider Advocate who works only with dental providers. Provider Advocates can be contacted according to the county where your office is located. Learn who the Provider Advocate is for your county.
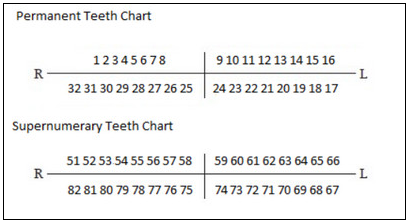
How are supernumerary teeth indicated on the patient's tooth chart in My Insurance Manager?
Supernumerary teeth are not indicated on the patient's tooth chart in My Insurance ManagerSM because the likelihood of someone having supernumerary teeth is so rare (less than 20 percent of the population). Refer to the chart below for the standard numbering scheme when reporting services rendered on supernumerary teeth in the permanent dentition. Add an "S" to the letter of the primary tooth corresponding to a supernumerary tooth in the primary dentition. Contact the appropriate service center if you have questions related to a member's benefits for services involving supernumerary teeth.
When filing claims for a Federal Employee Program (FEP) BlueDental member on an ADA claim form, should it go to BlueCross FEP Medical first?
Yes, submit all claims to the member's primary medical plan first. Primary payment will be sent to you, and then FEP Medical will forward the claim, along with the primary payment amount, to FEP BlueDental. The primary benefit will be coordinated on the claim received from the medical carrier and upon completion of coordination of benefits. FEP BlueDental will send the secondary payment to you.
Is the submission of a pre-treatment estimate similar to a prior authorization request?
A pre-treatment estimate is a real time snapshot of the benefits that are payable at the time the pre-treatment processes. It is considered a prior authorization. For Commercial dental plans, it is recommended but not required to request a pre-treatment estimate for services over $300.
What is a non-duplicate policy?
Non-duplication refers to coordination of benefits. This means that we coordinate up to our payment. We will not pay anything as secondary if the primary plan’s payment is equal to or greater than our primary payment. For example: If a dentist charges $62.00 for a filling (D2140) and the allowed amount is $60.00, we will pay $0 if the other coverage pays $60.00. Another example: If the dentist is charging $70.00 for a perio-cleaning (D4910) and the allowed amount is $65.00, if the other carrier pays $45.00, then we will pay $20.00 ($65.00-$45.00=$20.00).
What is a missing tooth clause?
Services related to teeth missing prior to the member’s effective date of coverage with our dental plan are not covered.
Are there waiting periods applied to certain services?
Yes, some commercial dental plans apply a waiting period. This is dependent on the group’s benefits. Some plans may have no waiting period, while others may have waiting periods of 6-12 months, applicable to basic and major or just major.




















