What To Know About Health Insurance and Pregnancy

March 23, 2023
Having a baby is a thrilling event for many families. No one wants to have to think about health insurance during such an exciting time. There are ways BlueCross BlueShield of South Carolina can help.
“I like to call us the best kept secret. A lot of people don’t even know they have their insurance company as a resource during pregnancy,” says Marie Fox, a registered nurse and maternity program manager at BlueCross. “This is especially true for first-time parents who may not have had to use their benefits before.”
Here are few important things to know about pregnancy, birth and health insurance.
Ask questions.
Being ready for pregnancy and giving birth is important. Fox encourages people to ask questions.
“Asking questions and preparing for the birth of your baby will help ease frustration and decrease stress,” she says.
BlueCross is here to help.
BlueCross is a resource for pregnant women. You likely have questions. Reach out to our team for help.
“We can help members navigate their benefits,” Fox says.
The best way to reach someone is to call the number on the back of your BlueCross member ID card. If you don’t have a copy, you can find your ID card in My Health Toolkit® online or in the app. Different plans have different customer service teams. Calling the number on your card will get you to the correct team quickly. Find out more about the importance of your ID card on our blog.
Notify BlueCross when you can.
There are a lot of people to share your news with when you find out you are pregnant. You likely aren’t thinking about telling your insurance company. But letting your insurance company know as soon as possible will help with medical claims in the future.
When you do, our team will connect you with our maternity care program. The customer service team will make sure your doctor or chosen provider is in network.
This will help make sure we will cover your care. Out-of-network care costs more.
Enroll in a maternity coaching program.
BlueCross has a dedicated care team to support you during and after your pregnancy. The Maternity Care program is for eligible pregnant members. If you’re currently expecting, you may have already received an invitation to enroll and get started with the My Health Planner℠ app.
You can also access the program by logging in to the My Health Toolkit mobile app. Under Benefits, select My Health Planner and follow the instructions.
The program gives expecting mothers a direct line to a support team. They can even text nurses to ask questions throughout their pregnancies.
When you enroll, you will have access to an interactive program timed to your pregnancy. The program follows you through six weeks after you give birth.
All nurses in this program are trained in obstetrics. We also have nurses trained in the neonatal intensive care unit. They can help members who need specialized care.
The maternity coaching program helps members with:
- Postpartum depression screenings.
- Gestational diabetes.
- Educational resources.
- Finding social and behavioral health services.
“It takes a village. We are part of that. You are not expected to have all the answers,” Fox says. “Sometimes you just need extra support. We want to help you reach healthy outcomes for your entire family.”
Understand your coverage.
Each health plan is different. Contact your health insurance company early to understand your benefits and coverage.
Many OB-GYNs charge one fee for pregnancy. It includes all prenatal visits, delivery and postpartum care. You usually get the bill after you have your baby.
Insurance may not cover some care. Knowing this in advance will prevent surprise bills.
Care that is typically not covered includes:
- Ultrasounds that are not medically necessary.
- Out-of-network providers.
- Home births, midwives or doulas.
Your plan may cover some midwives and birthing centers if they work with in-network providers. Your health insurance company can help you understand what your plan does or does not cover.
Knowing your benefits will also help you decide what plan to add your child to after he or she is born. Planning for this ahead of time will limit stress later.
Many plans include a breast pump.
The maternity care team can help you order a breast pump through insurance. Fox suggests ordering a pump before you deliver your baby so you can take it to the hospital with you.
It can be helpful to have the lactation consultant or nurse show you how to use your breast pump.
After the baby is born, new parents will likely have more questions about their insurance. Find important information on adding your child and other details on our blog.
If you have questions, reach out to customer support or the maternity care team. BlueCross is here to help.
Related Reading
 What To Know About Health Insurance and Childbirth
What To Know About Health Insurance and Childbirth
Having a baby is a thrilling event for many families. No one wants to have to think about health insurance during such a momentous time. There are ways BlueCross can help. Here are some important things to know about having a baby and using your health insurance.
Read More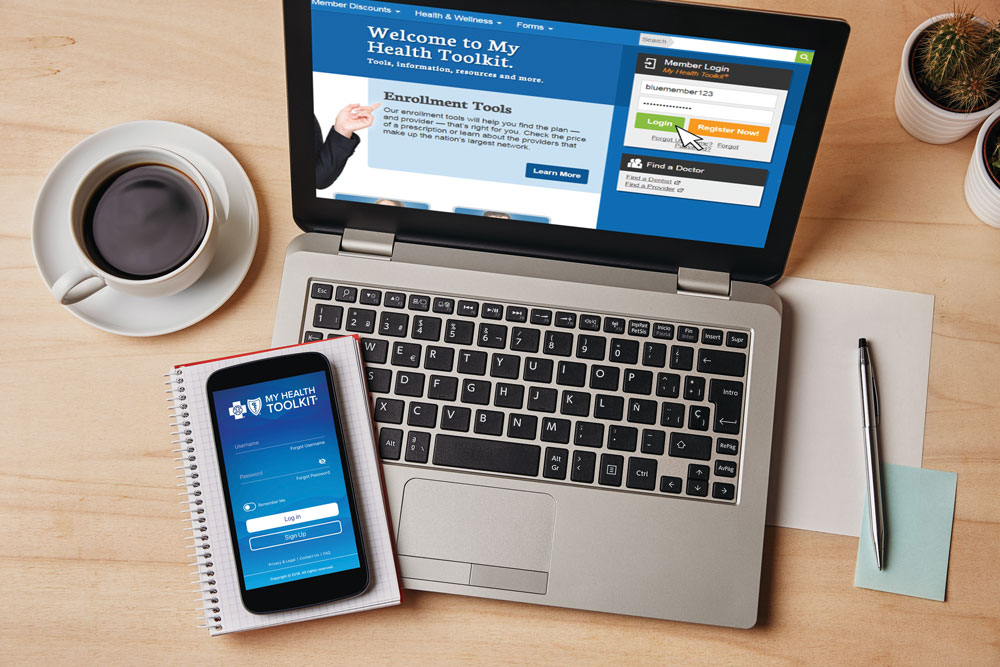 What To Know About ID Cards
What To Know About ID Cards
Some of the most common questions members ask our customer service team center around ID cards. Here are important things everyone should know about their ID cards.
 9 of Your FAQs Answered
9 of Your FAQs Answered
Every day our customer service advocates answer calls from members with questions about their health plans. Many of the answers to the most frequently asked questions can be found on BlueCross’s online portal, My Health Toolkit®.
Read More



















